HOW SENSEMEDIC AND COLLABREE JOIN FORCES TO SUPPORT PATIENTS TO ESTABLISH STICKY HABITS AND IMPROVE PATIENT OUTCOMES
Summary
Poor medication adherence affects about 50% of all patients with a chronic disease. This not only leads to suboptimal patient outcomes but also burdens our healthcare systems with additional and avoidable costs. Moreover, in Europe alone, around 200,000 people die each year because they do not follow their therapy plan as prescribed.
The increasing digitization and possibilities of smart and connected devices opens up new opportunities to support patients in making the necessary behavioral changes and to sustainably improve their adherence to therapy.
This white paper gives insights on how Sensemedic and Collabree combine their expertise to address the problem of poor treatment adherence.
“Increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments.”
World Health Organization, 2003
Lack of medication aderence: A global and costly problem
Adherence to a medication regimen is defined as “the extent to which patients take their medications as prescribed by their healthcare providers.”[1]
Poor adherence or non-adherence to medications includes all patients who do not commence their prescribed therapy at all, discontinue it prematurely, or take their medications in doses or frequencies different from the prescribing clinician’s recommendations. The treatment of chronic illnesses commonly includes the long-term use of pharmacotherapy. Although these medications are effective in combating disease, their full benefits can often not be realized, as approximately 50% of all patients with chronic conditions do not take their medications as prescribed[2]. To put this into perspective, even though it is well known that antidiabetics, antihypertensive, and lipid-lowering medication therapies can significantly reduce the risk of ischemic events[3] [4] [5], long-term adherence to these medications is poor even among patients who have already experienced a cardiovascular event[6]. For example, even though pharmacological antihypertensive therapy has a positive safety and tolerability profile and reduces the risk of stroke by approximately 30% and myocardial infarction by approximately 15%[5], evidence from a number of studies suggests that as many as 50% to 80% of patients treated for hypertension are non-adherent to their treatment regimen[7].
In general, non-adherence leads to poor disease control with a burden on patient quality of life and healthcare systems[8], whereas patients who take their prescribed medications regularly are more likely to enjoy better health outcomes, avoid complications and premature death and use less of emergency care and inpatient hospital services[9].
Medication non-adherence leads to premature deaths as well as an increased use of healthcare services. In the United States, between USD 100 and USD 300 billion of avoidable health care costs and approximately 125,000 deaths have been attributed to nonadherence per year[10] [11]. These estimates do not include avoidable costs of long-term care, diagnostic testing and pharmacy costs related to therapy intensification. Broader societal costs of increased disability, reduced productivity, and sick leave are also not considered[10].
With regards to Europe, it is estimated that non-adherence contributes to nearly 200,000 premature deaths per year[9] and costs European governments EUR 125 billion annually in excess healthcare services[12]. Diabetes, hypertension and hyperlipidaemia appear to give rise to the highest avoidable costs. Among patients with these three conditions, it has been estimated that between 4% and 31% do not fill their first prescription. Of those who do fill their prescription, only 50% to 70% take their medications regularly (i.e. at least 80% of the time)[9]. Ever since the WHO report on adherence was published, a large number of interventional studies have been conducted, but adherence rates have not noticeably improved[13] [14].
Sensemedic and Collabree set out to reimagine adherence interventions
Sensemedic increases medication adherence via smart reminding. Sensemedic was introduced in 2007 and has since been used in many projects where it has contributed to improving the adherence of participating patients.
Sensemedic is a product of Evalan, an innovation company based in Amsterdam, The Netherlands. Evalan develops, markets, and sells services that use state-of-the-art communications technology, with focus on remote monitoring and “Internet of Things” solutions. To support the delivery of these services, Evalan develops mobile devices and sensor units, data management systems, data processing algorithms and user interfaces on various platforms. In addition to Sensemedic, Evalan developed products like bGrid, SmartEagle, ARMOR and BACE, some of which have spun out into separate companies. Evalan works in cooperation with international technology partners and universities, and executes projects for industrial companies, hospitals, and research organizations. The cooperation with Collabree aligns with Evalan’s objectives to support progress in areas that matter for Europe, like healthcare, sustainability and food production.
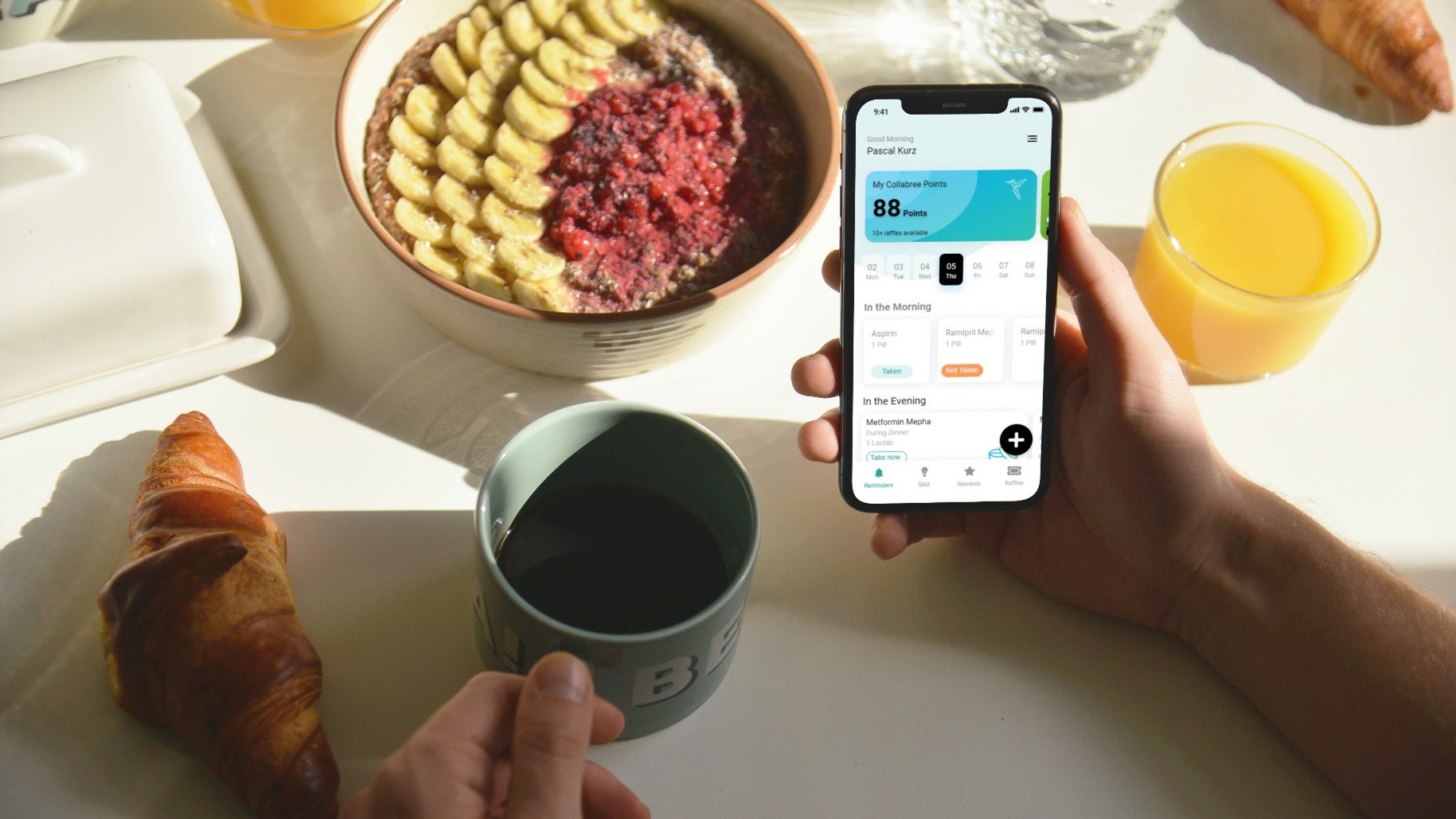
“With our adherence intervention, we rely on Sensemedic’s expertise to accurately monitor medication adherence, and we are excited by their ability to respond flexibly to our needs. We are convinced that the combination of our intervention with Sensemedic’s smart devices can lead to a significant improvement in patient outcomes.”
Pascal Kurz, CEO Collabree AG

Collabree is a digital adherence start-up focusing on improving therapy compliance of chronically ill patients by applying behavioral economics principles. Collabree believes in behaviorally-inspired interventions to increase medication adherence. Such interventions need to consider key behavioral drivers to design more effective remediations for non-adherence. There are several underlying decision errors that contribute to challenges patients face in forming healthy behavioral change. An example of such a decision error and a significant behavioral driver attributed to medication non-adherence is present bias. Present bias is the tendency for people to discount larger future rewards and prefer smaller immediate rewards[15].
Collabree’s strategy to overcome present bias is to provide a short-term reward for increased medication adherence. These external rewards can provide motivation to supplement insufficient intrinsic motivation for behaviors. These motivational instruments include contingent rewards, gamification and instant feedback and visualization of progress. This will help kickstart behavioral change and form long-lasting habits.
“Innvations such as Collabree’s novel intervention are needed to improve medication adherence. Technology can support this innovation and demonstrate that it is effective when implemented at scale.”
Henk Schwietert, CEO Evalan BV
Connected devices meet digital intervention in a clinical trial
Collabree currently tests efficacy and safety of the novel intervention to improve medication adherence in a clinical trial in Switzerland at the University Hospital in Basel (ClinicalTrials.gov Identifier: NCT04708756). The study is conducted as randomized controlled intervention study.
Next to Collabree’s digital intervention to improve medication adherence, a central element within this clinical trial is to accurately monitor the medication adherence of all included study participants. Within the trial, the smart Sensemedic pill dispensers are being used to monitor and documented the daily medication intake.
Sensemedic accurately determines the adherence of each patient in real-time and remotely. It works independently; the patient only needs to store his or her medication in a special Sensemedic dispenser, without having to connect the dispenser to a computer or an app. The medicine box is available in different sizes and has several compartments that are filled depending on the treatment.
Each time the patient opens the dispenser, a brief message is sent to a cloud application. The messages that are generated by the dispenser are sent wirelessly, through the cellular network. Each medication event that is registered by a dispenser is stored in the cloud application within about 20 seconds. This means that the patient’s adherence to therapy can be accurately determined.
The healthcare professional can view the data through the secure Sensemedic Web Portal, and thus guide and support the patient in a more targeted manner. For researchers the data set can be exported to allow further analysis.
With Sensemedic, it is also possible to remind patients to take their medicines with methods that use the real time measuring data. Thus, a patient can be reminded with a text message, whereby the text message is only sent when a patient forgets to take his or her medicine on the prescribed time.
Sensemedic works in nearly every country in the world at locations where mobile phones have network coverage. The dispenser makes it possible to monitor medication usage in real-time and supports moving existing behavior towards a better intake pattern and improved adherence.
Boost your patients’ outcomes with our solutions
Learn more about how Sensemedic and Collabree can help your patients with the difficult task of behavior change, establishing sticky habits, and monitoring therapy adherence accurately in real time.
Sensemedic and Collabree have an interesting solution for you. Get in touch here:
Henk Schwietert
CEO – Evalan BV
[email protected]
+31 (0)6-43559103
Pascal Kurz
CEO – Collabree AG
[email protected]
+41 (0)79 963 51 52
[1]: Osterberg, L. & Blaschke, T. Adherence to medication. New England Journal of Medicine 353, 487–497 (2005). [2]: World Health Organization. Adherence to long-term therapies - Evidence for action. (2003). [3]: Amarenco, P. & Labreuche, J. Lipid management in the prevention of stroke: review and updated meta-analysis of statins for stroke prevention. The Lancet Neurology 8, 453–463 (2009). [4]: Baigent, C. et al. Efficacy and safety of cholesterol-lowering treatment: Prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 366, 1267–1278 (2005). [5]: Law, M. R., Morris, J. K. & Wald, N. J. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ (Clinical research ed.) 338, b1665–b1665 (2009). [6]: Glader, E. L., Sjölander, M., Eriksson, M. & Lundberg, M. Persistent use of secondary preventive drugs declines rapidly during the first 2 years after stroke. Stroke 41, 397–401 (2010). [7]: Brown, M. T. & Bussell, J. K. Medication adherence: WHO cares? Mayo Clinic Proceedings 86, 304–314 (2011). [8]: Schroeder, K., Fahey, T. & Ebrahim, S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory settings. Cochrane Database of Systematic Reviews (2004) doi:10.1002/14651858.cd004804. [9]: Khan, R. & Socha-Dietrich, K. Investing in medication adherence improves health outcomes and health system efficiency. (2018). [10]: Iuga, A. O. & McGuire, M. J. Adherence and health care costs. Risk Management and Healthcare Policy 7, 35–44 (2014). [11]: Viswanathan, M. et al. Interventions to Improve Adherence to Self-administered Medications for Chronic Diseases in the United States: A Systematic Review. Annals of Internal Medicine 157, 785–795 (2012). [12]: European Comission; OECD. Health at a glance: Europe 2018 - State of health in the EU cycle. (2018). doi:10.1787/f222b050-mt. [13]: Naderi, S. H., Bestwick, J. P. & Wald, D. S. Adherence to drugs that prevent cardiovascular disease: Meta-analysis on 376,162 patients. American Journal of Medicine 125, 882-887.e1 (2012). [14]: Briesacher, B. A., Andrade, S. E., Fouayzi, H. & Chan, K. A. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28, 437–443 (2008). [15]: Wang, Y. & Sloan, F. A. Present bias and health. Journal of risk and uncertainty 57, 177 (2018).